Bursitis Of The Foot Pain Alleviation
Bursae are fluid-filled sacs that act as shock absorbers and cushions for our bones and tendons. There are two such sacs located on the back of your heel. The subtendinous calcaneal, also called retrocalcaneal bursa, is situated between the Achilles tendon and the heel bone (calcaneus). The subcutaneous calcaneal bursa, which is also referred to as the Achilles bursa, is found on the backside of the heel and Achilles. If either or both of these bursae become inflamed, the result is pain and tenderness.
Causes
There are several factors which can lead to a person developing retrocalcaneal bursitis. In athletes, especially runners, overtraining, sudden excessive increase in running mileage may lead to retrocalcaneal bursitis. Tight or ill-fitting shoes can be another causative factor as they can produce excessive pressure at the back of the heel due to restrictive heel counter. A person with an excessively prominent posterosuperior aspect of the heel bone (Haglund deformity) may also have a higher predisposition to retrocalcaneal bursitis. In such individuals, pain would be reproduced when the ankle goes into dorsiflexion.
Symptoms
A dull ache under the heel when not weight bearing. Sometimes severe pain when walking. Pain can increase after resting (sleeping or sitting) then standing and placing pressure on the area again. Throbbing under the heel. Swelling may be identified as a discernible lump under the heel. This is the swollen calcaneal bursa itself. Tingling under the heel as swelling affect the plantar nerves. Pains shooting into the foot or up the leg.
Diagnosis
The doctor will discuss your symptoms and visually assess the bones and soft tissue in your foot. If a soft tissue injury is suspected, an MRI will likely be done to view where and how much the damage is in your ankle. An x-ray may be recommended to rule out a bone spur or other foreign body as the cause of your ankle pain. As the subcutaneous bursa is close to the surface of the skin, it is more susceptible to septic, or infectious, bursitis caused by a cut or scrape at the back of the heel. Septic bursitis required antibiotics to get rid of the infection. Your doctor will be able to determine whether there is an infection or not by drawing a small sample of the bursa fluid with a needle.
Non Surgical Treatment
Podiatric Care may include using anti-inflammatory oral medications or an injection of medication and local anesthetic to reduce the swelling in the bursa. An injection may be used for both diagnosis and for treatment. When you go to your doctor, x-rays are usually required to evaluate the structure of your foot and ankle to ensure no other problems exist in this area. They may advise you on different shoewear or prescribe a custom made orthotic to try and control the foot structure especially if you have excessive pronation. Sometimes patients are sent to Physical Therapy for treatment as well. To aid in relief of pressure points, some simple padding techniques can be utilized. Most all patients respond to these conservative measures once the area of irritation is removed.
Prevention
Maintain proper form when exercising, as well as good flexibility and strength around the ankle to help prevent this condition. Proper stretching of the Achilles tendon helps prevent injury.
Can Hammertoes Cause Leg Pain
.jpg) Overview
Overview
Essentially, there's one consistent type of hammertoes, the condition in which your toes are contracted into a hammer or upside-down "V" shape. However, depending on its severity, hammertoe is characterized into two forms. Flexible hammertoe is hammertoe in which the joints of the toes are still moveable or flexible and can be treated with nonsurgical therapies. Rigid hammertoe is the more serious condition in which the joints' muscles and tendons have lost any flexibility and the contraction cannot be corrected by nonsurgical means. As a result, surgery is generally required to deal with the problem. This is why it's important to consult a physician as soon as the problem is recognized for the possibility of successful nonsurgical treatment.
Causes
While there are a number of causes, there aren't many specific risk factors for hammertoes, women tend to get these problems more than men, but they occur without rhyme or reason. Diabetics, however, are more likely to get a hammertoe if they have underlying nerve damage in the toes and feet.
 Symptoms
Symptoms
Well-developed hammertoes are distinctive due to the abnormal bent shape of the toe. However, there are many other common symptoms. Some symptoms may be present before the toe becomes overly bent or fixed in the contracted position. Often, before the toe becomes permanently contracted, there will be pain or irritation over the top of the toe, particularly over the joint. The symptoms are pronounced while wearing shoes due to the top of the toe rubbing against the upper portion of the shoe. Often, there is a significant amount of friction between the toe and the shoe or between hammertoe the toe and the toes on either side of it. The corns may be soft or hard, depending on their location and age. The affected toe may also appear red with irritated skin. In more severe cases, blisters or open sores may form. Those with diabetes should take extra care if they develop any of these symptoms, as they could lead to further complications.
Diagnosis
Most health care professionals can diagnose hammertoe simply by examining your toes and feet. X-rays of the feet are not needed to diagnose hammertoe, but they may be useful to look for signs of some types of arthritis (such as rheumatoid arthritis) or other disorders that can cause hammertoe.
Non Surgical Treatment
Your podiatrist may recommend one or more of these treatments to manage your hammer toes. Wear shoes with roomy toe boxes which don?t force your toes together. Exercises to stretch and strengthen muscles in the toes. Over the counter toe straps, cushions, and corn pads. Custom orthotic inserts. Toe caps or toe slings. In severe cases, surgery to release the muscles in the affected toes.
Surgical Treatment
he basis for hammer toe surgery most often involves removing s portion of bone within the toe, to reduce the joint contracture. Depending on the direction the toe is deviated, soft tissue procedures may be necessary along with pinning the toe with a surgical wire.
Hammer Toe Caused By Bunion
.jpg) Overview
Overview
There are two different types. Flexible hammertoes. These are less serious because they can be diagnosed and treated while still in the developmental stage. They are called flexible hammertoes because they are still moveable at the joint. Rigid Hammertoes. This variety is more developed and more serious than the flexible condition. Rigid hammertoes can be seen in patients with severe arthritis, for example, or in patients who wait too long to seek professional treatment. The tendons in a rigid hammertoe have become tight, and the joint misaligned and immobile, making surgery the usual course of treatment.
Causes
Ill-fitting shoes or a muscle imbalance are the most common causes of Hammer Toe. If there is an issue with a muscle in the second, third or fourth toes preventing them from straightening, Hammer Toe can result. If one of these toes is bent long enough in one position, the muscles tighten and cannot stretch out. Left untreated, surgery may be required. Women are especially prone to developing Hammer Toe because of their shoes. Hammer Toe results from shoes that don?t fit properly. Shoes that narrow toward the toe, pushing smaller toes into a bend position for extended periods of time. High heels that force the foot down into a narrow space, forcing the toes against the shoe, increasing the bend in the toe.
 Symptoms
Symptoms
A toe stuck in an upside-down "V" is probably a hammertoe. Some symptoms are, pain at the top of the bent toe when putting on a shoe. Corns forming on the top of the toe joint. The toe joint swelling and taking on an angry red colour. Difficulty in moving the toe joint and pain when you try to so. Pain on the ball of the foot under the bent toe. Seek medical advice if your feet regularly hurt, you should see a doctor or podiatrist. If you have a hammertoe, you probably need medical attention. Ask your doctor for a referral to a podiatrist or foot surgeon. Act now, before the problem gets worse.
Diagnosis
Most health care professionals can diagnose hammertoe simply by examining your toes and feet. X-rays of the feet are not needed to diagnose hammertoe, but they may be useful to look for signs of some types of arthritis (such as rheumatoid arthritis) or other disorders that can cause hammertoe. If the deformed toe is very painful, your doctor may recommend that you have a fluid sample withdrawn from the joint with a needle so the fluid can be checked for signs of infection or gout (arthritis from crystal deposits).
Non Surgical Treatment
A person with hammer toes will be asked to practice some exercises for their toes to regain average structure and movement. The exercises usually involve stretching and strengthening their toes. The person may attempt to pick things up off the floor using only their toes. They may also stretch their toes on a regular basis by hand to ease them into straightening out. Another example of a physical exercise specifically for a person's toes involves crumpling a towel with the toes. The towel can lie underneath the person's feet and the person can use their toes to scrunch up the towel as they perform simple tasks such as reading a hammertoe book or watching television.
Surgical Treatment
Several surgical procedures are available to the podiatric physician. For less severe deformities, the surgery will remove the bony prominence and restore normal alignment of the toe joint, thus relieving pain. Severe hammertoes, which are not fully reducible, may require more complex surgical procedures. Recuperation takes time, and some swelling and discomfort are common for several weeks following surgery. Any pain, however, is easily managed with medications prescribed by your podiatric physician.
 Prevention
Prevention
Prevention of a hammer toe can be difficult as symptoms do not usually start until the problem is well established. Wearing shoes that have extra room in the toes may help the problem or slow down its development.
Bilateral Hallux Valgus Interphalangeus
Overview
 The term "hallux valgus" or "hallux abducto-valgus" are the most commonly used medical terms associated with a bunion anomaly, where "hallux" refers to the great toe, "valgus" refers to the abnormal angulation of the great toe commonly associated with bunion anomalies, and "abductus/-o" refers to the abnormal drifting or inward leaning of the great toe towards the second toe, which is also commonly associated with bunions. It is important to state that "hallux abducto" refers to the motion the great toe moves away from the body's midline. Deformities of the lower extremity are usually named in accordance to the body's midline, or the line bisecting the body longitudinally into two halves. In more severe cases, the hallux continuing in the abductus fashion eventually either overlaps or underlaps subsequent lesser (small) toes especially the second (adjacent toe).
The term "hallux valgus" or "hallux abducto-valgus" are the most commonly used medical terms associated with a bunion anomaly, where "hallux" refers to the great toe, "valgus" refers to the abnormal angulation of the great toe commonly associated with bunion anomalies, and "abductus/-o" refers to the abnormal drifting or inward leaning of the great toe towards the second toe, which is also commonly associated with bunions. It is important to state that "hallux abducto" refers to the motion the great toe moves away from the body's midline. Deformities of the lower extremity are usually named in accordance to the body's midline, or the line bisecting the body longitudinally into two halves. In more severe cases, the hallux continuing in the abductus fashion eventually either overlaps or underlaps subsequent lesser (small) toes especially the second (adjacent toe).
Causes
A bunion is more common in women than men due to women wearing tighter fitting shoes. This condition can cause a variety of different soft tissue and bony complaints which may result in severe pain.
Symptoms
Pain or soreness. Inflamattion and redness. A burning sensation. Numbness on the side of the great toe. Other conditions which may occur secondary to bunions include calluses on the big toe, sore between the toes, ingrown toenails, and stiffness of the joint where the great toe attaches to the foot.
Diagnosis
Clinical findings are usually specific. Acute circumferential intense pain, warmth, swelling, and redness suggest gouty arthritis (see Gout) or infectious arthritis (see Acute Infectious Arthritis), sometimes mandating examination of synovial fluid. If multiple joints are affected, gout or another systemic rheumatic disease should be considered. If clinical diagnosis of osteoarthritic synovitis is equivocal, x-rays are taken. Suggestive findings include joint space narrowing and bony spurs extending from the metatarsal head or sometimes from the base of the proximal phalanx. Periarticular erosions (Martel sign) seen on imaging studies suggest gout.
Non Surgical Treatment
If overpronation is diagnosed early enough, the mechanics of the feet can be adjusted using a prescription orthotic. If orthotics are worn consistently, many major foot deformities can be avoided such as bunions. Early detection is of paramount importance. When a bunion progresses and cannot be controlled by an orthotic, surgical correction may be a consideration. Many advances in bunion correction allow for surgical intervention to make healing and return to normal activities much easier than use of traditional bunion surgery. 
Surgical Treatment
As mentioned above, with mild cases, the bone is cut close to the big toe joint and shifted over into a correct position. The cut bone is held in placed with one or two surgical screws. With this procedure, just the top of the bone is moved over and the bottom of the bone remains in the same place. This technique is called the Austin bunionectomy and refers to type of bone cut that will be made by the Surgeon. There is, however, a limit on how far one can move the bone over with this technique. Its is generally thought that the cut bone should only be moved over a distance equal to half the width of the bone. In somes the bone may be moved over further.
Prevention
Shop for shoes that possess a removable liner, or insole, and stand on the liner after you have removed it from your shoe. This is an effective method to see if your shoe is wide enough in the forefoot to accommodate your bunion. If your bunion and forefoot are wider than the insole, your shoe will squeeze and constrict your bunion and create the symptoms that define this health problem. The insole should also be wide enough to fully accommodate your big toe when it points outward, away from your other toes.
Over-Pronation Cause
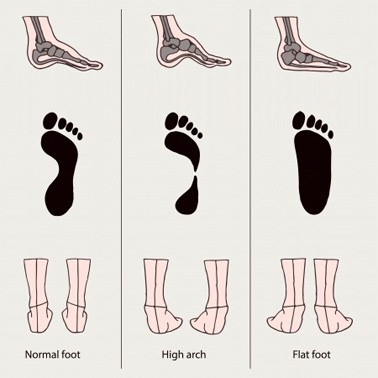
Overpronation is the most common abnormality found in the foot, and for this reason, is the most studied. The term that most people attribute to overpronation is ?flat feet.? Pronation is the rolling in of the foot and the collapse of the arch. Every person pronates to some extent and this is a necessary moment in the normal walking cycle as it allows the forefoot to make complete contact with the ground. Overpronation is when a person pronates too much and for too long. This places excess stress on the tendons and ligaments in the foot and ankle.

Causes
Over-pronation is very prominent in people who have flexible, flat feet. The framework of the foot begins to collapse, causing the foot to flatten and adding stress to other parts of the foot. As a result, over-pronation, often leads to Plantar Fasciitis, Heel Spurs, Metatarsalgia, Post-tib Tendonitis and/or Bunions. There are many causes of flat feet. Obesity, pregnancy or repetitive pounding on a hard surface can weaken the arch leading to over-pronation. Often people with flat feet do not experience discomfort immediately, and some never suffer from any discomfort at all. However, when symptoms develop and become painful, walking becomes awkward and causes increased strain on the feet and calves.
Symptoms
With over pronation, sufferers are most likely to experience pain through the arch of the foot. A lack of stability is also a common complaint. Over pronation also causes the foot to turn outward during movement at the ankle, causing sufferers to walk along the inner portion of the foot. This not only can deliver serious pain through the heel and ankle, but it can also be the cause of pain in the knees or lower back as well. This condition also causes the arch to sink which places stress on the bones, ligaments, and tendons throughout the foot. This may yield other common conditions of foot pain such as plantar fasciitis and heel spurs.
Diagnosis
At some point you may find the pain to much or become frustrated. So what are you options? Chances are your overpronation has led to some type of injury if there's pain. Your best bet is to consult with someone who knows feet. Start with your pediatrist, chiropodist or chiropractor. They'll be able to diagnose and treat the injury and give you more specific direction to better support your feet. One common intervention is a custom foot orthotic. Giving greater structural support than a typical shoe these shoe inserts can dramatically reduce overpronation.

Non Surgical Treatment
One of the best forms of treatment for over pronation is wearing supportive shoes. Shoes should have ample support and cushioning, particularly through the heel and arch of the foot. Without proper shoes, there may be additional strain on the tissue in the foot, greatly contributing to or causing an occurrence of over pronation. Rarely is surgery considered to relieve the pain and damage that may have resulted from this condition. Orthotic shoe inserts are often the easiest and most effective way to correct pronation.
Prevention
Duck stance: Stand with your heels together and feet turned out. Tighten the buttock muscles, slightly tilt your pelvis forwards and try to rotate your legs outwards. You should feel your arches rising while you do this exercise.
Calf stretch:Stand facing a wall and place hands on it for support. Lean forwards until stretch is felt in the calves. Hold for 30 seconds. Bend at knees and hold for a further 30 seconds. Repeat 5 times.
Golf ball:While drawing your toes upwards towards your shins, roll a golf ball under the foot between 30 and 60 seconds. If you find a painful point, keep rolling the ball on that spot for 10 seconds.
Big toe push: Stand with your ankles in a neutral position (without rolling the foot inwards). Push down with your big toe but do not let the ankle roll inwards or the arch collapse. Hold for 5 seconds. Repeat 10 times. Build up to longer times and fewer repetitions.
Ankle strengthener: Place a ball between your foot and a wall. Sitting down and keeping your toes pointed upwards, press the outside of the foot against the ball, as though pushing it into the wall. Hold for 5 seconds and repeat 10 times.
Arch strengthener: Stand on one foot on the floor. The movements needed to remain balanced will strengthen the arch. When you are able to balance for 30 seconds, start doing this exercise using a wobble board.
Calcaneal Apophysitis The Facts
Although the name might sound pretty frightening, Sever's disease is really a common heel injury that occurs in kids. It can be painful, but is only temporary and has no long-term effects. Sever's disease, also called calcaneal apophysitis, is a painful bone disorder that results from inflammation (swelling) of the growth plate in the heel. A growth plate, also called an epiphyseal plate, is an area at the end of a developing bone where cartilage cells change over time into bone cells. As this occurs, the growth plates expand and unite, which is how bones grow. Sever's disease is a common cause of heel pain in growing kids, especially those who are physically active. It usually occurs during the growth spurt of adolescence, the approximately 2-year period in early puberty when kids grow most rapidly. This growth spurt can begin any time between the ages of 8 and 13 for girls and 10 and 15 for boys. Sever's disease rarely occurs in older teens because the back of the heel usually finishes growing by the age of 15, when the growth plate hardens and the growing bones fuse together into mature bone. Sever's disease is similar to Osgood-Schlatter disease, a condition that affects the bones in the knees.
Causes
Sever?s is often present at a time of rapid growth in adolescent athletic children. At this time the muscles and tendons become tighter as the bones become larger. Between 8 - 15 years of age is the usual onset of this condition.
Symptoms
Symptoms of calcaneal apophysitis may include pain in the back or bottom of the heel, Limping, walking on toes, difficulty running, jumping, or participating in usual activities or sports. Pain when the sides of the heel are squeezed.
Diagnosis
The x-ray appearance usually shows the apophysis to be divided into multiple parts. Sometimes a series of small fragments is noted. Asymptomatic heels may also show x-ray findings of resporption, fragmentation and increased density. But they occur much less often in the normal foot. Pulling or ?traction? of the Achilles tendon on the unossified growth plate is a likely contributing factor to Sever?s disease. Excessive pronation and a tight Achilles and limited dorsiflexion may also contribute to the development of this condition.
Non Surgical Treatment
Cold packs: Apply ice or cold packs to the back of the heels for around 15 minutes after any physical activity, including walking.
Shoe inserts: Small heel inserts worn inside the shoes can take some of the traction pressure off the Achilles tendons. This will only be required in the short term.
Medication: Pain-relieving medication may help in extreme cases, but should always be combined with other treatment and following consultation with your doctor).
Anti-inflammatory creams: Also an effective management tool.
Splinting or casting: In severe cases, it may be necessary to immobilise the lower leg using a splint or cast, but this is rare.
Time: Generally the pain will ease in one to two weeks, although there may be flare-ups from time to time.
Correction of any biomechanical issues: A physiotherapist can identify and discuss any biomechanical issues that may cause or worsen the condition.
Education: Education on how to self-manage the symptoms and flare-ups of Sever?s disease is an essential part of the treatment.
Foot Arches Pain In Left Side
Arch pain is felt on the underside of your foot between the heel and ball. The purpose of the arch is to transfer your body weight from heel to toe, and pain is the result when the arch doesn?t function properly. Your foot actually contains two arches: the longitudinal arch which runs the length of your foot, and the transverse arch (also known as the metatarsal arch) which spans the width of your foot. There are 24 bones which create the arches and these bones are held together through their unique interlocking shapes and ligaments. The muscles and the plantar fascia (a broad band of fibrous tissue which runs from the heel to the toes) provide secondary support, and fat pads help to absorb impact and bear your weight. If any of these structures or their interaction are damaged or faulty, arch pain may occur. The most common cause of arch pain is plantar fasciitis, an inflammation of the plantar fascia. You may also suffer arch pain if you have a structural imbalance in your foot or suffer from arthritis. But arch pain may also result from stepping on a rock or when someone steps on your foot. This force may cause an injury such as a bone fracture or damage to the supporting muscles, ligaments, or tendons underneath your foot.

Causes
In most cases, plantar fasciitis develops without a specific, identifiable reason. There are, however, many factors that can make you more prone to the condition. Tighter calf muscles that make it difficult to flex your foot and bring your toes up toward your shin. Obesity. Very high arch. Repetitive impact activity (running/sports). New or increased activity.Although many people with plantar fasciitis have heel spurs, spurs are not the cause of plantar fasciitis pain. One out of 10 people has heel spurs, but only 1 out of 20 people (5%) with heel spurs has foot pain. Because the spur is not the cause of plantar fasciitis, the pain can be treated without removing the spur.
Symptoms
The primary symptom is pain or aching in the arch area. This can be accompanied by inflammation and tenderness. If the pain is caused by the plantar fascia, it is likely to be considerably more severe in the mornings due to the muscles being unused.
Diagnosis
To come to a correct diagnosis, your podiatrist will examine your foot by using his or her fingers to look for a lump or stone bruise in the ball of your foot. He or she will examine your foot to look for deformities such as high or low arches, or to see if you have hammertoes. He or she may use x-rays, MRIs (magnetic resource imaging), and CT scans to rule out fractures and damage to ligaments, tendons, and other surrounding tissues. Your doctor will also inquire about your daily activities, symptoms, medical history, and family history. If you spend a lot of time running or jumping, you may be at a higher risk for pain in the bottom of your foot. These diagnostic tests will help your doctor come to a proper diagnosis and create an appropriate treatment plan.
Non Surgical Treatment
Stretch the fascia. Prop your toes up against a wall, keeping your arch and heel flat so the toes stretch. Hold for a count of 10. Repeat 10 times three or four times per day. Roll a frozen water bottle under the arch. Stretch first then roll out the arch for 10 minutes; you don?t want to stretch the tendon when it?s ice cold. Freeze a golf ball and massage the fascia. Roll the frozen golf ball under the foot, starting from the front and working your way back. Put good pressure on each spot-the medial, center and lateral positions-for 15 seconds before moving to the next area. Then, roll the ball back and forth over the entire foot. Foam roll all muscles on the body above the plantar. Even tight shoulders can cause the condition, as your arm swing can throw off proper hip alignment and footstrike. Bump your arch. Get a commercial insole with an arch bump to push on the plantar and keep it from flexing-it doesn?t matter if you?re an under or overpronator; the plantar needs to be supported and strengthened, Wear the support in all shoes, if possible.
Surgical Treatment
In cases where cast immobilization, orthoses and shoe therapy have failed, surgery is the next alternative. The goal of surgery and non-surgical treatment is to eliminate pain, stop progression of the deformity and improve mobility of the patient. Opinions vary as to the best surgical treatment for adult acquired flatfoot. Procedures commonly used to correct the condition include tendon debridement, tendon transfers, osteotomies (cutting and repositioning of bone) and joint fusions.
Prevention
People who run regularly should replace shoes every six months, more frequently if an avid runner. Avoid running or stepping on uneven surfaces. Try to be careful on rocky terrain or hills with loose gravel. Holes, tree stumps and roots are problems if you are trail running. If you have problems with the lower legs, a dirt road is softer than asphalt, which is softer than concrete. Try to pick a good surface if possible. However, if you're racing, be sure to train on the surface you'll eventually run on. Be careful running too many hills. Running uphill is a great workout, but make sure you gradually build this up to avoid injuries. Be careful when running downhill too fast, which can often lead to more injuries than running uphills. Prevent recurrent injuries. Athletes who have experienced ankle injuries previously may benefit from using a brace or tape to prevent recurrent ankle injuries.